What is Keratoconus?
Keratoconus is a corneal disorder where the cornea (the front “windshield” of the eye) undergoes progressive thinning and steepening resulting in increased amounts of astigmatism and decreased best corrected vision.
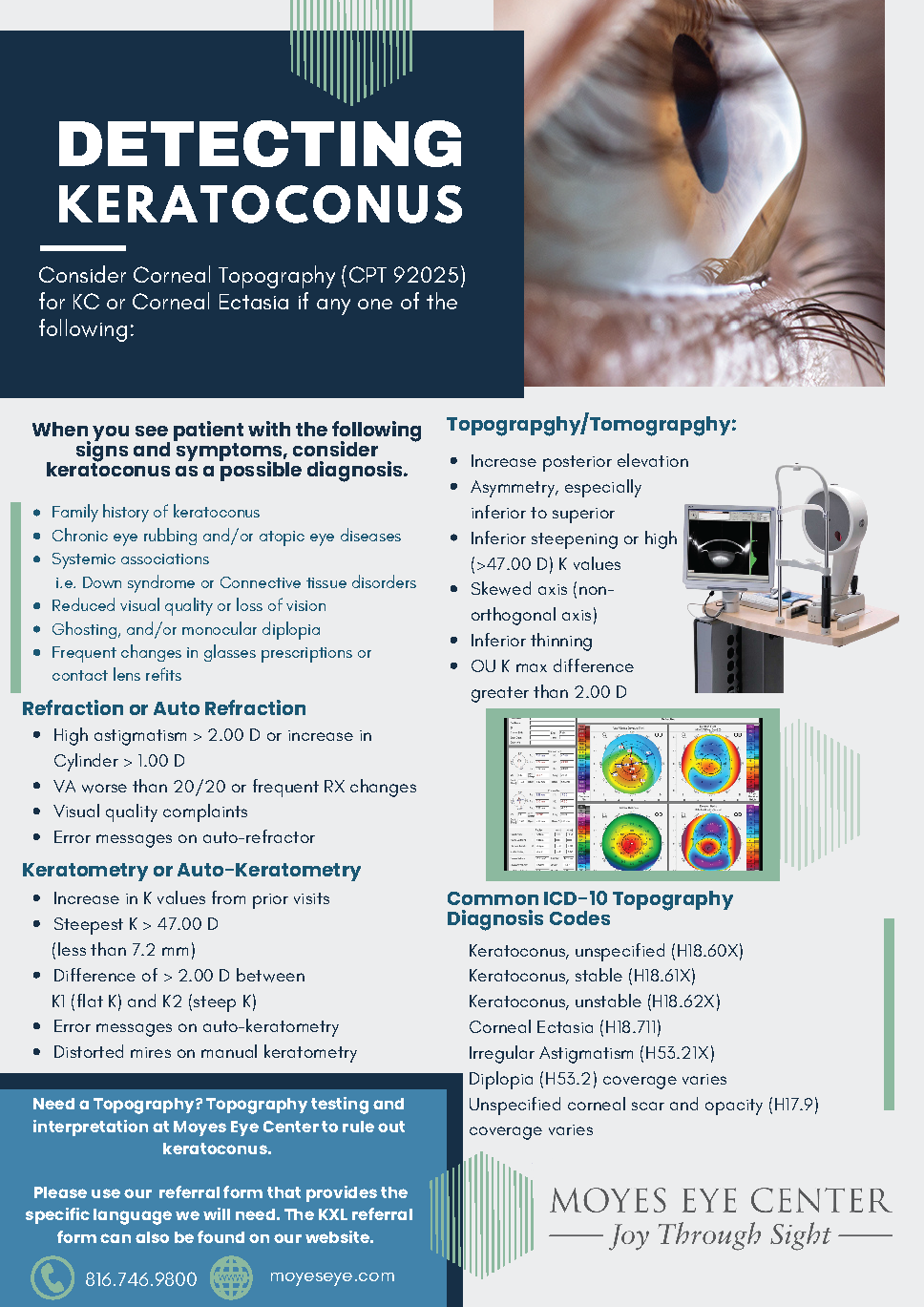
Normal Cornea
Keratoconic Cornea
Keratoconus affects 1 in 2000 people. Most cases involve both eyes, frequently in an assymmetric fashion. For many, keratoconus is very slowly progressive and vision remains very correctable with standard glasses or contact lenses. For some, keratoconus can be more rapidly progressive eventually leading to a need for surgical intervention to maintain good vision.
Symptoms
Progressively blurred vision
Increasing amounts of astigmatism or nearsightedness
Increasing difficulty to correct vision to 20/20
Diagnosis
The diagnosis of keratoconus is often delayed at first until vision is noticed to not be correctable to 20/20 and/or there is a large increase in astigmatism or nearsightedness between eye exams. Your doctor can perform a corneal topography or map of the shape of the cornea to detect early keratoconus.
Treatment
As it pertains to vision correction, early keratoconus is treated with glasses or contact lenses. Although initially soft contact lenses may work to achieve good vision, eventually rigid gas permeable or mini scleral contact lenses become necessary to correct the irregular corneal shape. If contact lenses becomes intolerable, surgical options can be discussed.
Patients with keratoconus that are showing signs of progression should be evaluated for Corneal Cross Linking (CXL). Signs of progression would be further reduction in vision, increase in astigmatism or nearsightedness and other clinical signs of corneal steepening.
Surgical options include corneal cross linking, intacs corneal ring segments, penetrating keratoplasty and DALK (deep anterior lamellar keratoplasty).
To learn more about keratoconus please visit the National Keratoconus Foundation at: https://www.nkcf.org/